Over 40% of the U.S. infantry reported chronic pain (defined as pain lasting over 3 months) after deployment, and 15% reported opioid use in the past month. [1] Like the civilian population, prescription opioid misuse is a concern for military personnel. The military has responded to this issue by implementing medication treatment for opioid use disorder (MOUD) in VA facilities. Historically, MOUD at the VA has been prescribed only through substance use disorder clinics and did not reach Veterans who were not seen in these clinics.
The Stepped Care for Opioid Use Disorder Train-the-Trainer (SCOUTT) Initiative
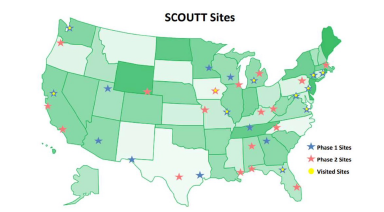
In order to expand access to MOUD, the Office of Mental Health and Suicide Prevention (OMHSP) launched the Stepped Care for Opioid Use Disorder Train-the-Trainer (SCOUTT) Initiative. The overarching goal of SCOUTT is to improve access to MOUD in primary care, pain management, and mental health clinics. SCOUTT began in the Spring of 2018 with successful implementation in 36 VA facilities nationwide. Since methadone is only available through licensed treatment programs, SCOUTT focuses on increasing prescribing of buprenorphine and injectable naltrexone. To increase MOUD prescribing in VHA primary care, mental health, and pain clinics, SCOUTT provided training to providers working in those settings on how to provide MOUD and facilitated its implementation by providing an ongoing learning collaborative. [2]
Implementation barriers to the SCOUTT Initiative included delays in credentialing, knowledge gaps, and provider and patient-related stigma. SCOUTT has worked to overcome these barriers, and MOUD is now available for Veterans at the following sites:
Implementing Stepped Care for Opioid Use Disorder Train the Trainer (SCOUTT) Initiative (VA)
Opioid Use Disorder and Post-Traumatic Stress Disorder
Substance abuse disorders are common among both civilians and military personnel with Post-Traumatic Stress Disorder (PTSD). Studies have shown that, among psychiatric conditions, PTSD is highly comorbid with substance use disorders, and the likelihood of developing PTSD are highest with OUD. [3] In fact, among individuals with OUD having a comorbid PTSD is associated with more severe addiction, higher rates of depression, attempted suicide, and psychosocial problems. [3] These results show the need to better identify PTSD among those with OUD, and to use brief, integrative treatments for both disorders in the clinic.
Treatments for Opioid Use Disorder with PTSD
Presence of PTSD in a patient with OUD requires closer monitoring for acute
acute psychiatric issues, including suicide. The first step towards is to provide the appropriate PTSD assessment for OUD treatment-seeking individuals. Once the diagnosis is made, it’s crucial to treat both disorders. Assessment tools and treatment options for PTSD can be found here:
https://www.ptsd.va.gov/understand_tx/tx_basics.asp
Treatment retention is often cited as a limitation of MOUD. However, studies show that participation in a PTSD-focused behavioral treatment improves treatment retention with MOUD. [4] Among Veterans, those with PTSD-diagnosed who received trauma treatment within 3-months of buprenorphine induction had much greater odds of remaining in buprenorphine at 6-months than those without trauma treatment. [5] Another study of PTSD-diagnosed veterans with chronic pain found twice as many veterans on buprenorphine, compared to other opioid medication, had improvements of their PTSD symptoms. [6]
[1]Toblin RL, Quartana PJ, Riviere LA, Walper KC, Hoge CW. (2014.) Chronic Pain and Opioid Use in US Soldiers After Combat Deployment. JAMA Intern Med. Jun 30.
[2] https://pubmed.ncbi.nlm.nih.gov/32697170/
[3] https://pubmed.ncbi.nlm.nih.gov/34182307/
[4] https://pubmed.ncbi.nlm.nih.gov/30243036/
[5] https://pubmed.ncbi.nlm.nih.gov/16562404/