The first few months of the State Targeted Response Technical Assistance (STR-TA) initiative provide insight into how much help is needed in local communities on the prevention, treatment and recovery of opioid use disorder. As a result, states and territories are responding to the STR-TA request center for innovative approaches to meet the need with the help of 417 consultants who are on board to lend their assistance to the effort locally.
The STR-TA grant, funded by the Substance Abuse and Mental Health Services Administration and led by the American Academy of Addiction Psychiatry with a coalition of national professional organizations, is providing local expertise and technical assistance to better prepare the healthcare and general community in confronting this public health crisis. By using resources such as Providers Clinical Support System’s trainings, Addiction Technology Transfer Center, BRASS TACS, to name a few , the initiative’s goal is to provide local technical assistance (TA) in the most cost-effective and efficient way possible while building sustainability.
 As soon as the STR-TA website was launched, requests for technical assistance started coming in. As of mid-July, 142 requests for TA had been requested via the STR-TA website. But further review indicated these requests actually represent close to 1,000 requests as most requests had several additional requests per submission. By August 1, STR-TA anticipates having received 175 request submissions from across the country.
As soon as the STR-TA website was launched, requests for technical assistance started coming in. As of mid-July, 142 requests for TA had been requested via the STR-TA website. But further review indicated these requests actually represent close to 1,000 requests as most requests had several additional requests per submission. By August 1, STR-TA anticipates having received 175 request submissions from across the country.
The key to the success of the STR-TA project is getting the word out to healthcare systems, state agencies, individual prescribers, all health professionals, recovery and prevention communities, and the general public that STR-TA is ready and willing to provide expertise at the local level. We wanted to share one example of what one state is doing as a result of STR-TA request.
STR-TA Consultant Maher Karam, MD, an Addiction Psychiatrist in Harris County, Texas, and others on the Texas STR-TA team came up with an aggressive plan to contact every prescriber in Texas who has applied to the DEA for a waiver to prescribe buprenorphine and ask if they need technical assistance in educational resources, clinical mentorship, or training that would help them in being better prepared and comfortable with treating these patients. Drs. Karam and Tom Kosten, along with other prescribers in Texas, have agreed to convene bi-weekly calls with any provider in Texas who might have clinical case questions or answer questions they may have.
The main focus now is getting the word out to communities across the country and five U.S. territories, that TA is available. Research suggests that only 20% of clinicians who have obtained their waiver to prescribe medications for treating opioid use disorders (OUD) prescribe. Providers cite a variety of reasons why they do not prescribe, including: 1) uncomfortable with managing addiction in general, 2) lack of staff trained to provide support, 3) no infrastructure or system within their clinical practice to handle SUD, 4) lack of access to behavioral health, and 5) stigma around treating patients with OUD. By contacting these prescribers personally by a local addiction specialist, Dr. Karam hopes to identify those who wish to treat OUD, but for some reason are not. The next step will be to determine what TA is needed to address any barriers facing clinicians and their patients.
The task is not a small one. In Harris County alone, 257 clinicians are waivered and in the state of Texas, 1,207 clinicians are waivered far few are prescribing, Dr. Karam said. Dr. Karam along with his colleagues Drs. Kosten, Daryl Shorter and others are motivated to make it happen and in a big TEXAS way.
“People are overdosing and dying. It’s not about avoiding abuse, it’s about avoiding death,” Dr. Karam said, noting the urgency of the crisis. “If we can get 10 percent of the 257 providers who are waivered but not prescribing to start prescribing, we will have made a good start.”
Around the country, other TA consultants at the local level are getting the word out about the STR-TA grant and the many resources and support by providing TA in conferences, presenting at local meetings, inviting colleagues to shadow them in their practice, by answering colleagues questions in an one-on-one setting or on a weekly discussion group on a phone call discussing clinical cases.
When a state, territory, healthcare system, or individual practitioner makes a TA request, they are contacted within 24 hours for more information. From there, a local technology transfer specialist (TTS) assigned to that state/territory is contacted to determine if he or she can address the request. Of requests submitted thus far, 24% were submitted by states/territories/STR grantees and the remaining 76% were from individuals, healthcare systems, treatment providers, medical and primary care associations, and other community organizations.
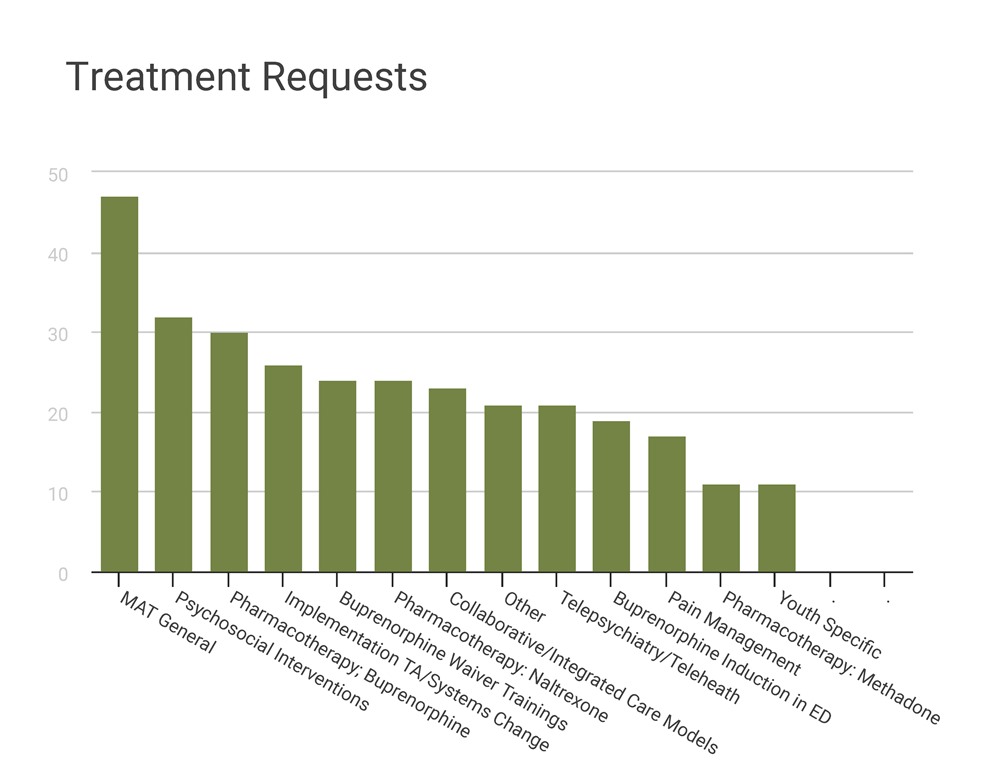
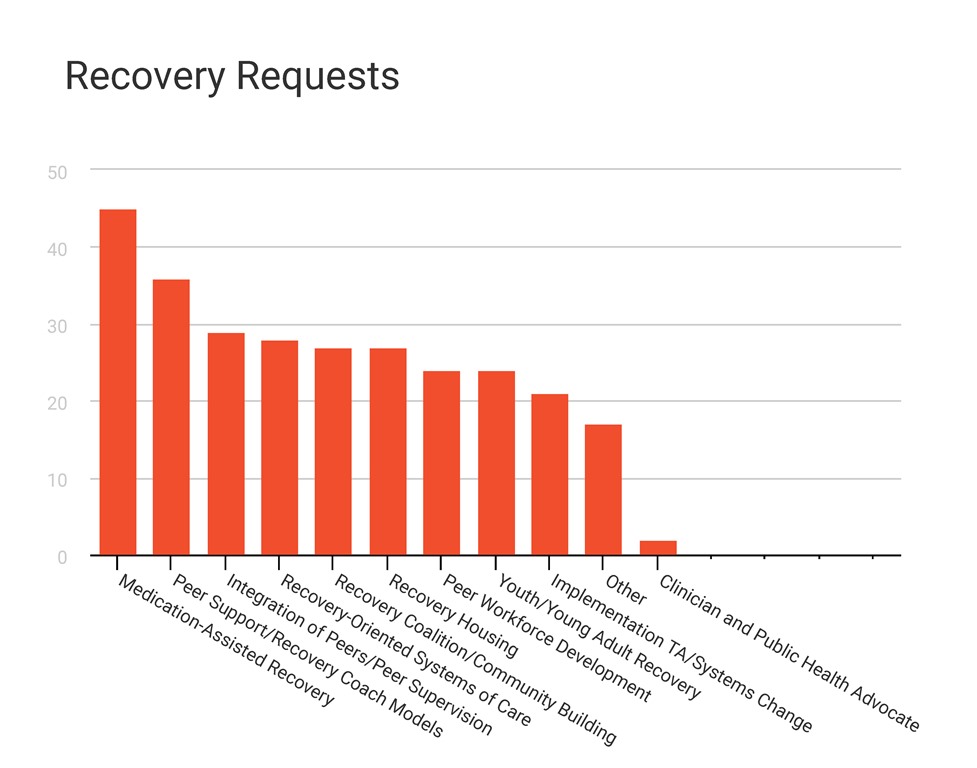
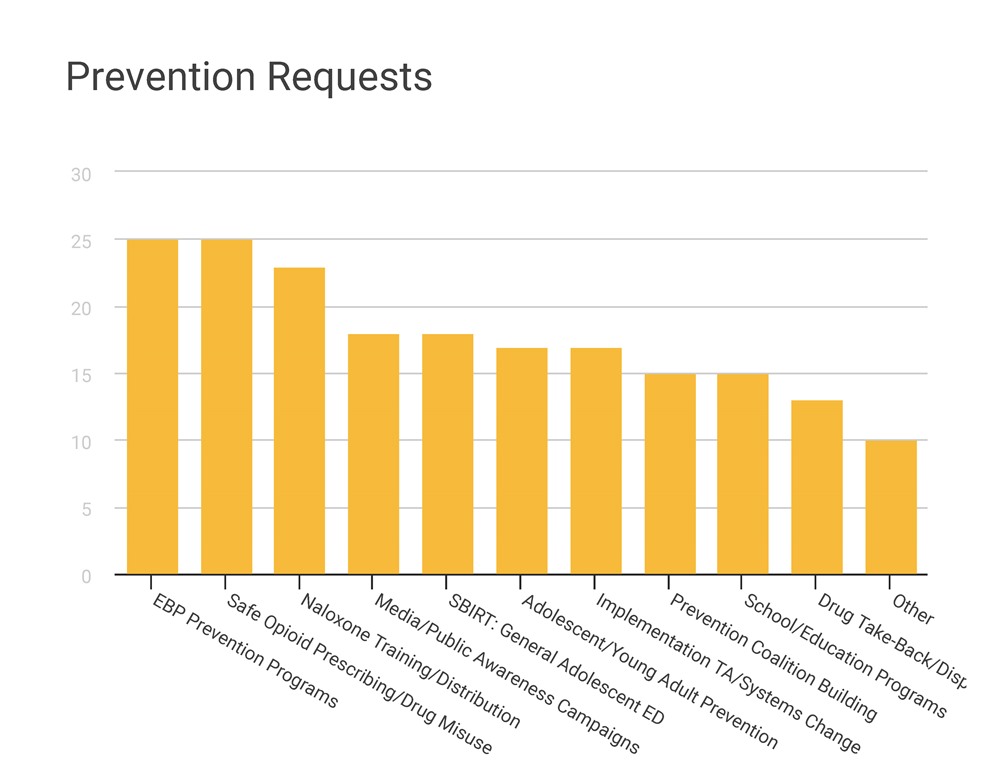
The requests have been coming in for all areas—prevention, treatment, and recovery—and encompass a wide range of issues (see charts below). TA services provided include:
- Building a coalition
- Conduct educational meetings
- Conduct local consensus discussions/stakeholder engagement/strategic planning
- Conduct needs assessment
- Develop and facilitate, a formal implementation plan
- Distribute educational materials/resources
- Provide a training (build specific skills)
- Map local resources (identify champions, community leaders, waivered providers, treatment programs, etc.)
- Organize clinician implementation team meetings
- Program marketing
- Provide ongoing consultation (mentoring or clinical coaching sessions)
Thus far, STR-TA has made major strides in a short time. We have clinical, recovery and prevention consultants ready to help meet local needs in addressing the OUD crisis.
Let us know what you need.
For more information about the STR-TA initiative, go to www.getSTR-TA.org.